How can compression therapy benefit wound care patients?

Chronic wounds are wounds that do not heal in a predictable amount of time like most wounds. What exactly constitutes a predictable amount of time is highly variable, since there is no clear consensus, with current medical literature stating this ranges between 4 weeks and 3 months [1].
Regardless of healing time, chronic wounds represent a growing medical and socio-economic problem that places a huge burden on healthcare professionals and healthcare programmes which have to divert resources from other, possibly more important, prevention and management programmes for other diseases. The statistics are worrisome and are becoming graver with each newly published study.
Chronic wounds statistics
For example, just for the United States, a 2009 study presented a number of 6.5 million for patients with chronic wounds [2]. A newer study from 2018 presented the far higher number of 8.2 million [3]. This number only encompasses those patients who are Medicare beneficiaries (14.5 % of all beneficiaries according to the 2014 data set) and not all individuals who might be affected, are beneficiaries of other medical insurance programmes or are without any medical insurance [3].
Medicare spent between $28.1 billion and $31.7 billion on treatment of (all types of) wounds in 2014 alone [3]. Of this a significant amount was for the treatment of chronic wounds. More specifically, $2.08 billion ($2.15 billion is the mid-range estimate) was spent on the treatment of arterial ulcers (ischaemic ulcers) and $0.72 billion ($0.78 billion is the mid-range estimate) on the treatment of venous wounds (including associated infections) [3].
Disparity in treatment costs between arterial and venous wounds is even more pronounced when the costs are calculated by wound type per beneficiary. Treatment of arterial ulcers cost $9,105 per beneficiary, while the treatment of venous wounds carried a price tag of $1,138 or $1,252, if the treatment cost of associated infections is added [3].
The situation is no better in other developed nations. One UK study estimated that, at any given time, there are at least 190,000 individuals in the UK with venous leg ulcers, but researchers note that, due to the methodology used and limited scope of available data, that number is probably far higher [4]. The cost of chronic wound management is also likely to be grossly underestimated, with some estimating the cost to the NHS (National Health Service) being between £2.3 and £3.1 billion for care for patients with chronic wounds per year (at 2005/2006 prices) [5].
However, even more worrying than the ambiguous number of patients and the cost of treatments, is the fact that many patients were not given a comprehensive diagnosis of their ulcers and even didn’t receive any treatment. A comprehensive survey of wound care in the UK found that 40 % of patients with leg ulcers had either not received the recommended ankle-brachial (pressure) index (ABPI or ABI) assessment or it was unclear whether a recording had been taken [6]. Around 31 % of patients with venous leg ulcers were not receiving compression therapy [6].
Significant treatment costs, in addition the growing prevalence of chronic wounds, were also identified in Germany. It is estimated, on the basis of medical data for 9 million beneficiaries of statutory health insurance (GVK), that about 0.7 % of insured patients were affected with leg ulcers [7]. Of the costs, one study gives an estimation of €9,569 for treatment per ulcer per patient [8]. These costs are projected to increase in the future for a variety of reasons, including an aging population – not just in Germany or the UK – but worldwide. The national healthcare systems should therefore be well prepared and relevant diagnostic and treatment guidelines should be set up that improve the quality of diagnosis of patients with lower-extremity ulcers. One way of achieving this is through the general and conscientious utilisation of ABI measurements.
Three simple steps towards correct wound assessment
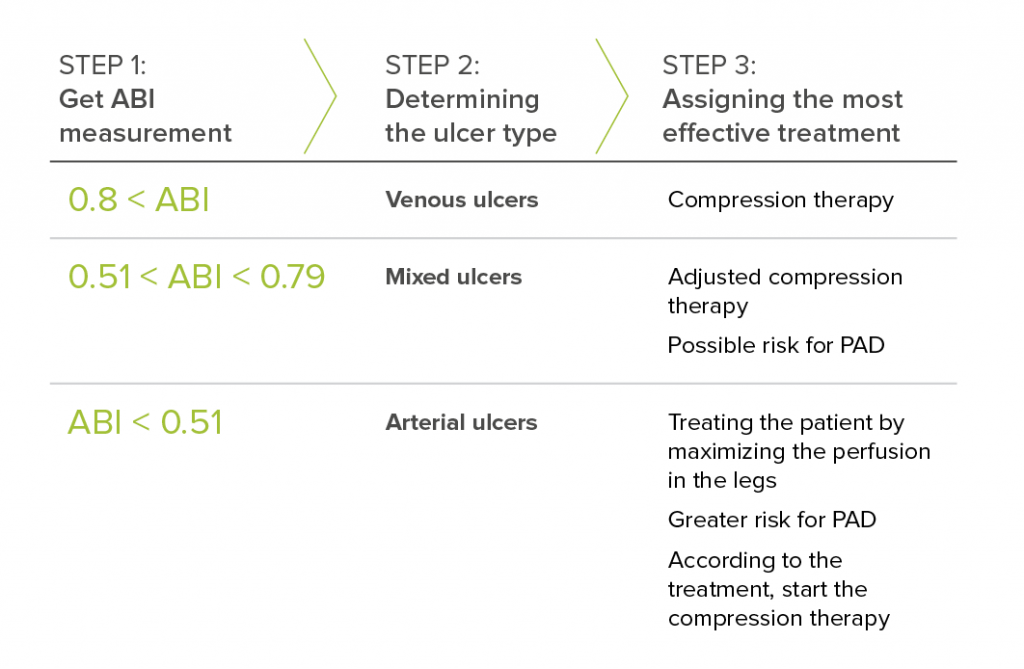
Types of Ulcers & Recommended Treatment
Venous ulcers are treated with compression therapy. Before any compression therapy is undertaken, a clinician should determine the level of compression that can be safely applied to a specific leg. For this the ABI result (ABI 0.8 – 1.20 and above) is key, not only from a wound assessment perspective but also from a legal point of view.
Mixed ulcers are defined by an ABI between 0.79 and 0.51, which means they can be treated with compression therapy but with reduced pressure because there is also a risk of PAD.
Arterial ulcers are also associated with an ABI under 0.5, which means that an examined patient most likely has PAD. Arterial ulcers cannot be treated with compression therapy. Their healing potential can be greatly improved if they are properly diagnosed and medical staff educate patients on maximising perfusion in legs impaired due to PAD [9].
The Importance of Ankle-Brachial Index (ABI)
ABI measurement is the first and most important step in chronic wound assessment, as it helps clinicians differentiate between types of ulcers and make better treatment choices. This has been recognised by many healthcare organisations around the world that tirelessly raise awareness about the importance of correct wound assessment.
That’s where we are trying to make a contribution by giving clinicians the best tool for the job - MESI ABPI MD®. The fact that its being rapidly adopted by general practitioners and wound care specialists worldwide is not only a testament of its usability, but a sign that we are on the right path.
Looking for MESI ABPI MD?
Meet its smarter successor – the MESI mTABLET ABI. This wireless, 4-cuff solution brings ABI measurement into the era of integrated diagnostics. Part of the modular MESI mTABLET platform, it delivers a 1-minute PAD assessment and expands with other diagnostic tools to fit your clinical needs.
Contact sales