Monitoring Patients after Operative Procedures


Peripheral Artery Disease (PAD) is a complex and serious cardiovascular disease (CVD), but like many (but not all) CVDs, it can be effectively managed using conservative methods so long as the condition is diagnosed in a timely manner. This is most easily achieved through an ABI or TBI assessment, which have, particularly the latter, diagnostic applications that are beyond those connected with PAD.
In 2010 there were at least 202 million patients with PAD (or LEAD, Lower Extremity Artery Disease, as it is increasingly also referred to as) – that number increased to 236.62 million in 2015 and today, in light of this rising trend, the prevalence is likely even higher, primarily due to ageing of the population and an increase in several important risk factors [1, 2]. However such worrisome estimates don’t really translate into numbers of definite diagnoses, as PAD is far more likely to be asymptomatic (40 % of patients) than symptomatic (10 % of all cases) or is ‘masked’ by other, unrelated medical conditions (atypical pain felt by the remaining half of patients) [3, 4]. Basing diagnosis solely on the presence of overt symptoms (intermittent claudication) or (unreliable) physical examination is foolhardy at best and bordering on malpractice as there are far better diagnostic methods available [5].
The Ankle-Brachial (Pressure) Index (ABPI or ABI) assessment is a prime example as it offers a level of accuracy and specificity in comparison with other, far more expensive methods (i.e. angiography). Cost-efficiency is coupled with the time-saving nature of the procedure (speed of assessment), particularly if performed with an oscillometric-plethysmographic diagnostic device in lieu of Doppler probe/sphygmomanometer combination [6, 7, 8]. But, despite its usability, particularly in general practice settings, it is greatly underutilised, even in at-risk patients. A comprehensive study of patients receiving wound care in the UK found that about 40 % of patients with lower-extremity ulcers had either not received an ABI assessment or it was unclear whether a recording had been taken – significant chance they might have been given inappropriate treatment [9].
Complications and the adverse outcomes of PAD are numerous and their severity greatly depends on timeliness of diagnosis and the presence of comorbid diseases, whether they are cardiovascular in nature or of another etiology/pathophysiology, with diabetes mellitus being a good example. This metabolic disorder is rapidly growing in prevalence (projected to affect at least 629 million individuals by 2045) and is also responsible for preventing accurate diagnosis of PAD (using ABI) in many patients through its contribution to the calcification (hardening) of arteries [10, 11].
Incompressible arteries can also be found in individuals with renal insufficiency and rheumatoid arthritis [12, 13]. Although toe arteries are rarely affected by calcification, they can be used as substitutes for blood pressure at dorsalis pedis/posterior tibial artery in the Toe-Brachial Index (TBI) assessment [14]. Additionally, like ABI, TBI has a diagnostic value beyond diagnosing PAD and even has an application in postoperative monitoring of vascular surgery patients and predicting the possibility of adverse outcomes in beneficiaries of revascularisation surgery.
3 Reasons Why TBI Is Important for Proper Recovery
Nearly any type of vascular surgery carries with it a substantial risk of adverse outcomes, particularly if major blood vessels are involved. Introduction and refinement of percutaneous procedures has mitigated (in patients that are suitable candidates for such procedures) many of possible complications associated with open surgery (for respective conditions) [15, 16, 17]. There remains a greater risk of complications still persisting in high-risk patients of an advanced age with comorbid cardiac and/or renal issues [18]. Comprehensive postoperative monitoring of vascular patients is therefore a must and should also include the use of ABI and TBI assessments, which have an added diagnostic value if performed as a part of preoperative screening.
The initial reason for TBI usage in the preoperative assessment of vascular surgery patients, both in lieu of PAD (in individuals with incompressible arteries) or due to other inherent benefits, is its prognostic value in wound healing potential. More specifically, it is the component of TBI, the Toe Pressure (TB), that is used in this particular assessment. A study that encompassed 333 amputations over a 5-year period found a clinically significant (positive) association between a TB of 47 mmHg (and above) measured before amputation and during postoperative wound healing [19]. This association held true even in the presence of confounding factors such as advanced age, chronic kidney disease (CKD) and concomitant revascularisation [19].
The secondary reason is predicting the possibility of adverse outcomes in patients with Critical Limb Ischaemia (CLI) during the post-revascularisation period. The most severe form of PAD is associated with a significant risk of amputation (in 10 % to 40 % of diagnosed patients in the 6-month period) and subsequent mortality (20 % in the 6-month period and up to 50 % for 5-year period) [20, 21, 22, 23, 24]. The severity of CLI and the risk of lower-extremity amputation/mortality is particularly pronounced in patients with comorbid PAD and diabetes (50 % to 76 % of patients with CLI are diabetics) [25, 26, 27]. Those patients are also more likely to have incompressible arteries, thus necessitating the use of TBI. The superiority of TBI and its component TB in predicting the likelihood of Major Adverse Limb Events (MALE) following revascularisation in such patients is well-researched and supported by ample evidence [28, 29, 30].
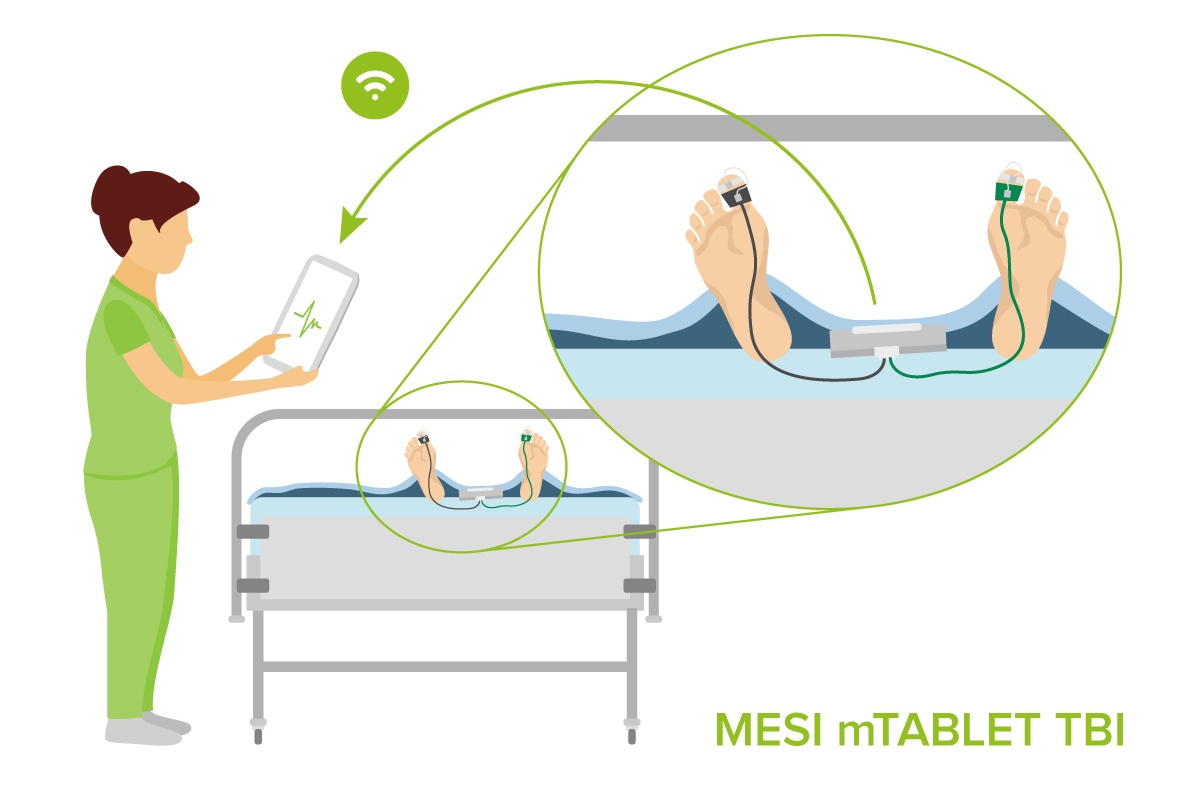
The third, and most important benefit of TBI, is the post-operative monitoring of vascular patients for signs of Acute Limb Ischaemia (ALI) due to thrombosis or embolism (or other reasons). Limb perfusion assessment is usually carried out using a Doppler probe and a sphygmomanometer (essentially an ABI measurement), although this may be difficult in those with incompressible arteries or with patients who have had a distal bypass (a risk of bypass thrombosis) [31, 32]. The TBI is a more versatile choice, especially if measured using a diagnostic device with integrated support for Electronic Health Records (EHRs). The EHRs have numerous benefits in comparison to traditional (paper) health records, in this case instantaneous entry of TBI result and fast and easy sharing of data with a vascular surgeon if there is a need for a thrombectomy/embolectomy or any other emergency procedure [33, 34, 35, 36, 37].
The TBI is a valuable tool for the perioperative assessment and monitoring of vascular surgery patients, particularly those with incompressible arteries or other conditions that preclude the use of an ABI assessment.