The Effect of Diabetes on Ankle-Brachial Index (ABI)
Diabetes affected an estimated 425 million individuals worldwide in 2017 and there is a strong indication that this number will continue to rise. Amongst its many complications and adverse health effects it also greatly increases the risk of a number of Cardiovascular Diseases (CVDs), including Peripheral Artery Disease (PAD) [1].
The mechanisms of the detrimental effects of diabetes (both type 1 and type 2) on cardiovascular health are complex and multi-faceted. Atherosclerosis is the dominant issue on a macrovascular level with metabolic changes associated with diabetes the main culprit as they lead to changes in the form and size of Low-density Lipoprotein (LDL) cholesterol and augment their atherogenic potential [2].
On a microvascular level, this mechanism is different and connected with Diabetic Autonomic Neuropathy (DAN), which damages the body’s autoregulation system (primarily the endothelial cells) of blood flow, resulting in the diminished flow of oxygen and nutrients to tissues [2,3]. Additionally, many diabetics often have other comorbidities, such as obesity, hypertension (prevalence rate of 30 % for type 1 and 60 % for type 2) and dyslipidaemia, which increase the risk of CVDs [4,5].
Why is Diabetes a Critical Risk Factor for Peripheral Arterial Disease (PAD)?
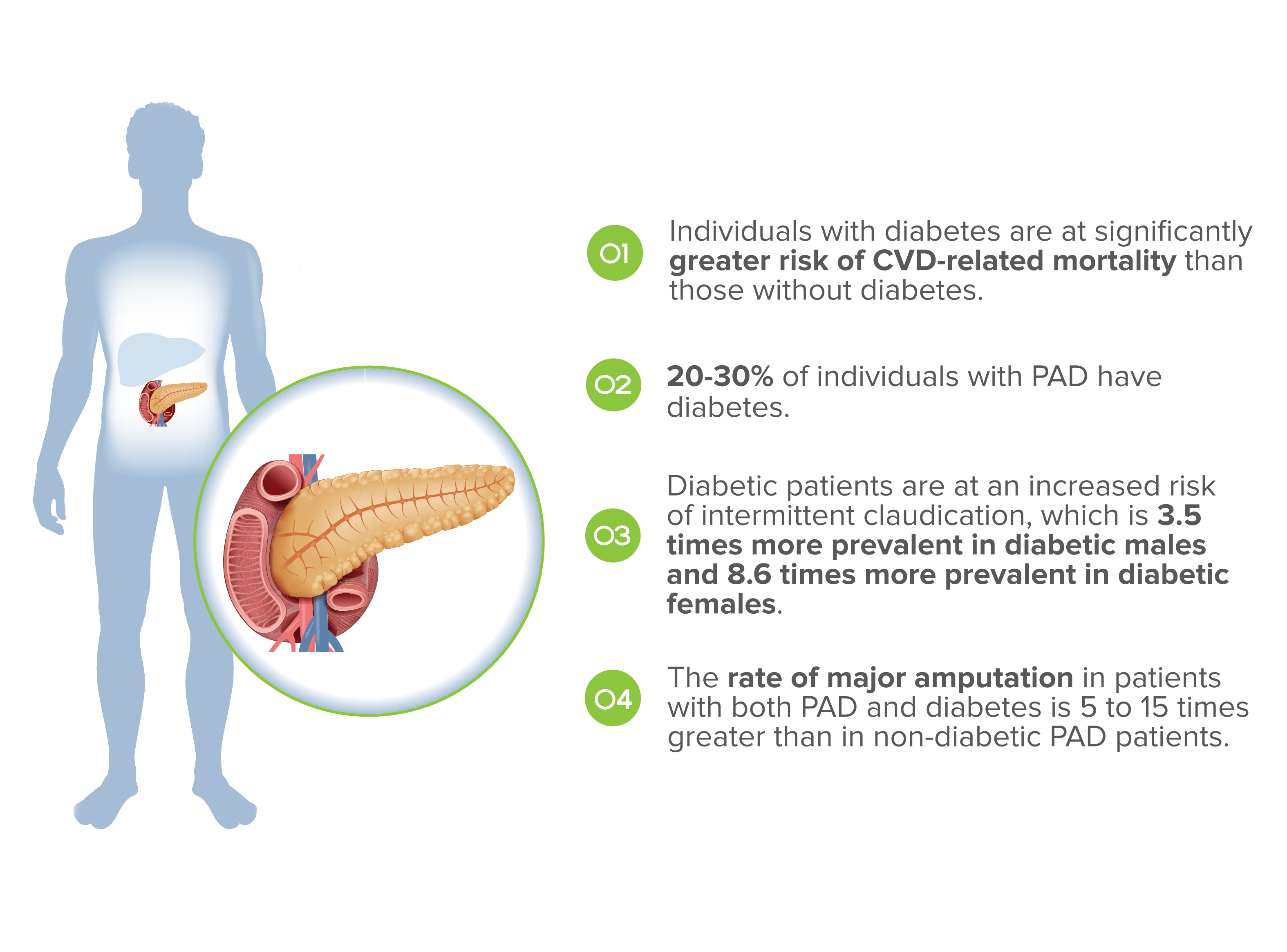
In general, individuals with diabetes are at significantly greater risk of CVD-related mortality (the most prevalent cause of mortality in diabetic population) than those without diabetes. Those with type 1 are at 4.2 times a greater risk of death and those with type 2 are at a 2 to 10 times greater risk of death [6]. Regarding PAD specifically, studies have indicated that glucose intolerance is associated with a greater than 20 % prevalence of an ABI (Ankle-brachial Index, one of the best indicators for PAD) in comparison with 7 % in individuals with normal glucose tolerance [7].
Approximately 20 to 30 % of individuals with PAD have diabetes, but this prevalence is likely to have been underestimated due to the often asymptomatic nature of PAD and altered pain perception due to diabetes-induced peripheral neuropathy [8].
And this is the single greatest risk of properly diagnosing PAD in those with diabetes: missing tell-tale signs of PAD due to diabetic peripheral neuropathy (namely intermittent claudication). Diabetic patients are at an increased risk of intermittent claudication, which is 3.5 times more prevalent in diabetic males and 8.6 times more prevalent in diabetic females (in comparison with non-diabetic populations for each gender) [9].
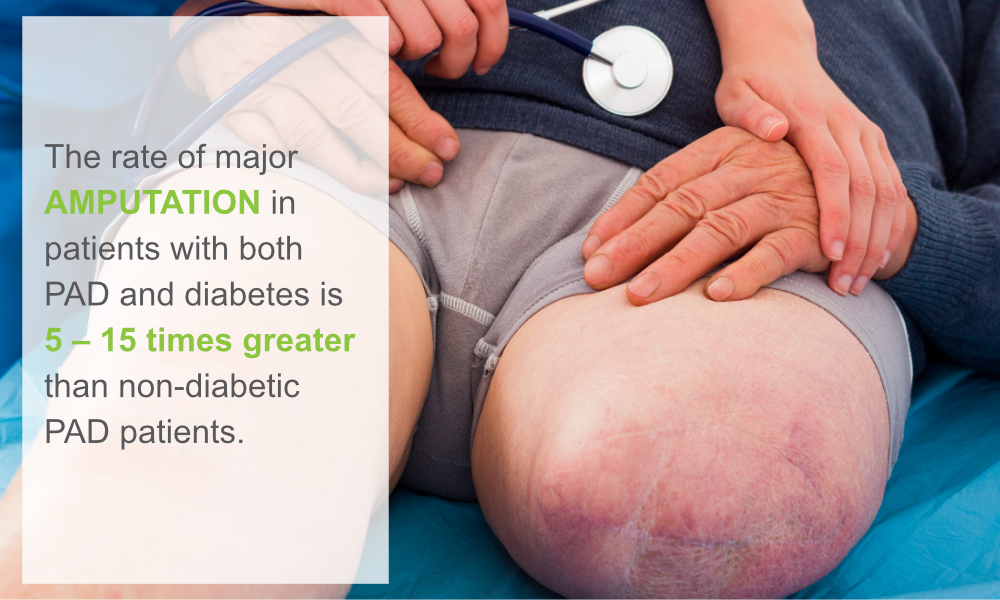
Only timely diagnosis on the basis of an ABI measurement can lead to proper care and management of PAD which can, if left untreated, lead to complications that manifest in far greater frequency and severity in diabetic patients. Specifically, the rate of major amputation in patients with both PAD and diabetes is 5 to 15 times greater than in non-diabetic PAD patients [7]. One of the complications of advanced stage PAD are ulcers on the lower extremities and about half of all diabetic patients with ulcers also have PAD [10].
Screening diabetic patients for PAD on the basis of Ankle-Brachial Index (ABI) is therefore not only recommended, but a necessity, if we wish to treat diabetes holistically.