Vascular health during the COVID-19 pandemic
Pandemics usually have an unprecedented effect on the social, economic and political fabric of our societies and the current COVID-19 pandemic is no exception. Nationwide lockdowns, remote working and learning, and social distancing coupled with mandatory protective mask wearing, new challenges for some industries and significant growth in others, and political instability are just some of the hallmarks of these troubling times.
The most significant has been the impact on healthcare systems which, by and large, have proved unprepared for the influx of patients with COVID-19 and the resource-intensive management of their symptoms. However, their travails may not be over anytime soon, not just because of COVID-19, but due to the likely growing number of patients (with cardiovascular issues) who are the indirect casualties of the current pandemic.
In this blog you will learn:
What are the health effects of confinement during the COVID-19 pandemic?
Does physical inactivity lead to deep vein thrombosis?
Why are compression therapy and ABI assessment important?
What are the health effects of confinement during the COVID-19 pandemic?
The health effects of prolonged confinement as experienced by many who were forced to remain indoors as a part of national lockdowns or as self-isolation due to confirmed or suspected COVID-19 infection are multifaceted and range from psychological to emotional and physiological. However, not all are equally affected nor to the same extent, but it should be noted that even primary school-aged children and elite athletes are not spared [1, 2]. The potential health issues of the latter are of more indirect nature—higher rates of injury due to detraining brought by prolonged confinement and associated physical inactivity [2].
We are, of course, more interested in the direct health consequences such as depression and anxiety and physiological changes brought by physical inactivity and other lifestyle factors. There is ample evidence that the incidence and severity of the aforementioned conditions and many others were significantly higher during the confinements. Disease pandemics in general are associated with an increase in prevalence of depression, stress, insomnia, post-traumatic stress disorder (PTSD), anger and burnout, and the few studies done on the current COVID-19 pandemic have demonstrated it is no exception [3-7].
A Spanish study on the psychological effects of confinement on students and staff of the University of Valladolid noted that from one fifth to nearly a third of responders reported moderate to extremely severe scores for anxiety, depression and stress [8]. Another, far more comprehensive meta-study that encompassed individuals from 17 countries around the word echoed these findings and highlighted that the detrimental (psychological) effects were more pronounced in those with pre-existing medical conditions or confirmed COVID-19 infection and in healthcare workers like (female) nurses [9]. Also of interest is a study that looked at changes in physical activity frequency, sleep duration, and alcohol consumption and smoking rates of Australians during the pandemic [10]. Not surprisingly given the intimate connection of aforementioned factors with psychological well-being (despite the study reporting no significant changes in psychological distress, although that may be due to the timing of data collection, lesser severity of lockdown and cultural factors), the study reported an increase in unhealthy practices [10].
These findings are also pertinent to the question of physical health, particularly the cardiovascular component, which will be discussed later on. However, it is not the only such study. An international online study encompassing more than a thousand participants from various countries around the world (primarily from Asia, Africa and Europe) compared their lifestyles before and during the confinement [11]. Just as in the Australian study, the surveyed individuals reported a decrease in physical activity and an increase in eating more unhealthy food [11], factors that are conducive to increased risk of cardiovascular diseases (CVDs) and greater chance of adverse outcomes in those who already have them.
Does physical inactivity lead to deep vein thrombosis?
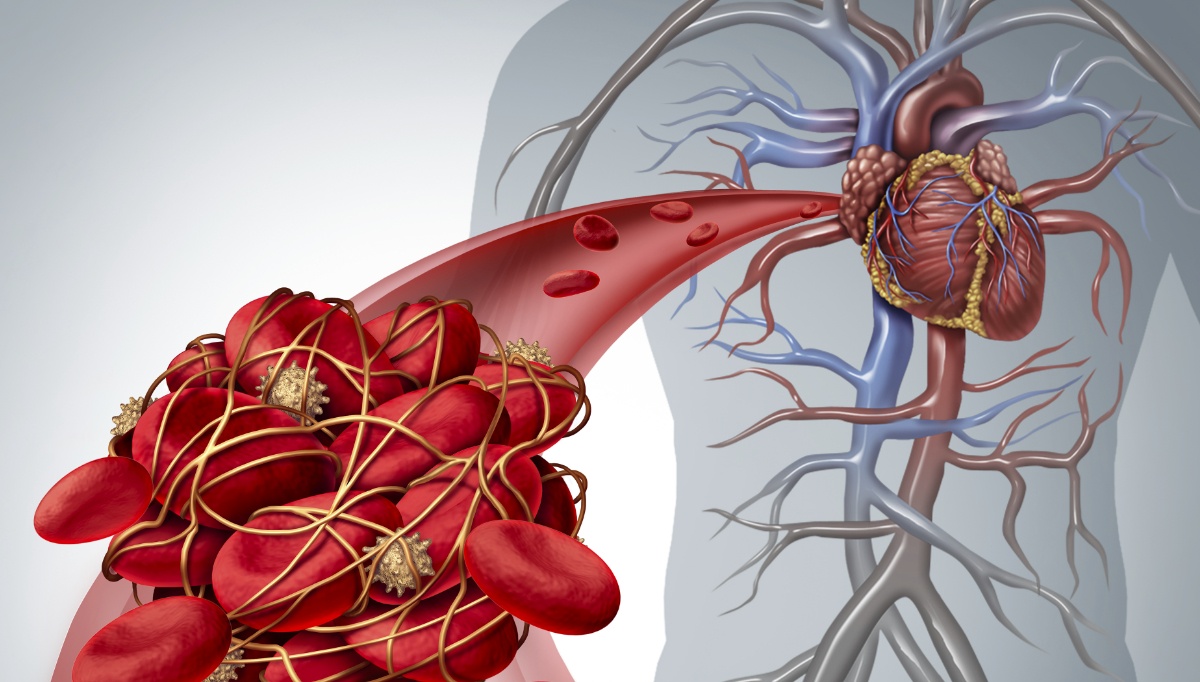
The association between physical (in)activity, unhealthy dietary habits that are often connected with obesity and type 2 diabetes, tobacco smoking, and higher incidence of CVDs is undisputed and well-researched [13-16]. Deep vein thrombosis (DVT) is, unfortunately, no exception, although the relative “contribution” of specific risk to greater incidence and disease severity is different from other CVDs.
Focusing just on the lack of physical activity, a comprehensive meta study (on venous thromboembolism – VTE, not DVT specifically, but given the connectedness of both conditions findings for one are at least partly applicable to the other) of 14 separate studies found that regular physical activity was significantly associated with lower risk of VTE in comparison with sedentary or less active lifestyle [17].
Given the fact that prolonged confinement has a negative effect on the frequency and intensity of physical exercise, what steps should those at risk of DVT and, even more importantly, those already diagnosed undertake to manage their symptoms? Apart from engaging in physical exercise, which can reduce acute symptoms and may help to prevent or improve post-thrombotic syndrome, those merely at risk should, of course, make more comprehensive lifestyle changes [18].
Why are compression therapy and ABI assessment important?
One of the most well-known conservative management tools for mitigating DVT symptoms (leg pain) and other issues connected to venous insufficiency is compression therapy (stockings, intermittent pneumatic compression, etc.) and with good reason [19, 20]. Nonetheless, it should only be used in patients with a known ABI (Ankle-Brachial Index) score to avert possible complications arising from undiagnosed peripheral artery disease (PAD) [21]. Underlying PAD limits or entirely precludes application of compression therapy.
An ABI assessment is, therefore, a prerequisite before deciding on starting compression therapy. The reality is often different; one study conducted in the UK found that a significant number of patients, up to 40%, with lower-extremity ulceration had not received an ABI assessment and nearly a third of those with venous ulcers were not receiving compression therapy [22]. There are several reasons for this and other (unpublished) lapses, including likely a lack of training and experience measuring ABI using a Doppler probe and a sphygmomanometer (for a long time the most common method), leading to false results [23]. Fortunately, there are newer tools, like oscillometric-plethysmographic diagnostic devices, that enable fast and user-error free ABI assessment and should be available at every healthcare facility that offers compression therapy [24, 25].
Prolonged confinement as a part of COVID-19 lockdowns is associated with significant detriments to psychological, emotional and physical well-being and may increase the rates of specific cardiovascular diseases like deep vein thrombosis. Proper and timely management using conservative measures like compression therapy guided by ABI assessment should follow a positive diagnosis as soon as possible.